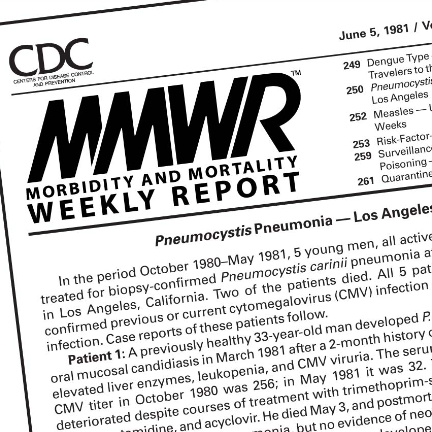
 On June 5, 1981, Morbidity and Mortality Weekly Report, the Centers for Disease Control and Prevention’s weekly report, included an article about five young gay men in Los Angeles treated for a rare form of pneumonia. This syndrome became known as gay-related immune deficiency, which would later be called acquired immunodeficiency syndrome, or AIDS, caused by the human immunodeficiency virus, or HIV.
On June 5, 1981, Morbidity and Mortality Weekly Report, the Centers for Disease Control and Prevention’s weekly report, included an article about five young gay men in Los Angeles treated for a rare form of pneumonia. This syndrome became known as gay-related immune deficiency, which would later be called acquired immunodeficiency syndrome, or AIDS, caused by the human immunodeficiency virus, or HIV.
During the past 40 years, HIV/AIDS has impacted millions of men, women, and children across the globe. According to UNAIDS, since the start of the pandemic, an estimated 75.7 million people have acquired HIV, and 32.7 million people have died from AIDS-related illnesses. However, with the development of effective HIV treatment and prevention options such as antiretroviral therapy, or ART, and pre-exposure prophylaxis, or PrEP, the United Nations reports AIDS-related mortality rates have dropped 42 percent and new HIV infections by 29 percent since 2010. Presently, approximately 38 million people globally are living with the virus, with many maintaining full lives.
Since its inception in 1999, the HPTN has successfully designed and implemented complex clinical research studies focusing on biomedical interventions and integrated strategies to prevent HIV acquisition and transmission.
With more than 85 research sites in 19 countries and more than 50 clinical trials ongoing or completed, reported HPTN study findings with crucial public health and policy impacts include:
- HPTN 052, the first randomized clinical trial to show that treating individuals living with HIV with ART early in their HIV infection (CD4 cell count 350-550/mm3) reduces the risk of sexual transmission of HIV to their partners not living with the virus. These landmark findings led to immediate changes to the World Health Organization’s treatment guidelines for when to initiate ART, including ART use in serodiscordant couples, as well as new guidance issued by the Office of Global AIDS Coordinator for programs supported by the PEPFAR program. Further analysis of HPTN 052 also demonstrated the cost-effectiveness of early ART.
- HPTN 061, the most extensive research study of Black men who have sex with men (BMSM) in the United States and the first to determine the rate of new HIV infection among such a large prospective cohort of U.S. BMSM.
- HPTN 071 (PopART), a research study that examined the impact of a package of HIV prevention interventions on community-level HIV incidence in South Africa and Zambia. The prevention interventions included universal voluntary HIV counseling and testing provided at the household level, linking people living with HIV to care, and early initiation of antiretroviral therapy (ART) for all those living with HIV. Findings show delivery of an HIV prevention strategy that includes offering in-home HIV testing to everyone, with immediate referral to HIV care and treatment for people living with HIV based on prevailing in-country guidelines, can substantially reduce new HIV infections. According to projections from mathematical modeling and cost-effectiveness analyses, a continuation of community-wide HIV testing and prompt initiation of treatment as delivered in the study could lead to substantial reductions in new HIV cases, be cost-effective, and help to achieve the UNAIDS 2030 targets.
- HPTN 083, a study comparing the efficacy and safety of long-acting injectable cabotegravir (CAB-LA) to Truvada® for prevention of HIV acquisition in cisgender MSM and transgender women who have sex with men in North and South America, Asia, and South Africa. Data from the HPTN 083 clinical trial showed that a pre-exposure prophylaxis (PrEP) regimen containing long-acting cabotegravir (CAB LA) injected once every eight weeks was superior to daily oral tenofovir/emtricitabine (TDF/FTC) for HIV prevention among cisgender men and transgender women who have sex with men.
- HPTN 084, a study comparing the efficacy and safety of long-acting injectable cabotegravir (CAB-LA) to Truvada® for prevention of HIV acquisition in women in sub-Saharan Africa. Data from the HPTN 084 study indicated that a pre-exposure prophylaxis (PrEP) regimen of long-acting cabotegravir (CAB LA) injections once every eight weeks was safe and superior to daily oral tenofovir/emtricitabine (FTC/TDF) for HIV prevention among cisgender women in sub-Saharan Africa.
- Antibody-Mediated Prevention (AMP) are two studies that evaluated the safety and efficacy of VRC01, a broadly neutralizing monoclonal antibody (bnAb), in reducing acquisition of HIV-1 infection among cisgender men and transgender persons (TG) who have sex with men in North and South America, and Europe. (HVTN 704/HPTN 085), and sexually active cisgender women in sub-Saharan Africa (HVTN 703/HPTN 081). Findings from the proof-of-concept AMP studies demonstrated VRC01 effectively prevented the acquisition of HIV strains that were sensitive to the bnAb.
The HPTN also has long-standing partnerships with pharmaceutical companies such as Gilead Sciences and ViiV Healthcare, academic researchers worldwide, the Bill and Melinda Gates Foundation, and several other vital organizations. In addition, the HPTN has forged collaborations to develop integrated strategies with PEPFAR, the Centers for Disease Control and Prevention, and both ministries and departments of health in several countries.
The U.S. National Institute of Allergy and Infectious Diseases, the U.S. National Institute of Mental Health, Office of The Director, the U.S. National Institute on Drug Abuse, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, all part of the U.S. National Institutes of Health, co-fund the HPTN. Of course, the work of the HPTN would not be possible without the commitment of so many around the world, from research teams, study participants, funders, community partners, and other key stakeholders. In addition, the work of the HPTN would not be possible without the commitment of so many around the world, from research teams, study participants, funders, community partners, and other key stakeholders.
While we have come a long way since the earliest days of the pandemic, much remains to be done. Looking ahead, HPTN investigators, research staff, and community advocates from around the world remain enthusiastic about the potential for identifying new biomedical tools and strategies for the prevention of HIV transmission. If successful, various populations will garner the benefits of integrated HIV prevention strategies to control the HIV pandemic, helping reach the “end of AIDS.”